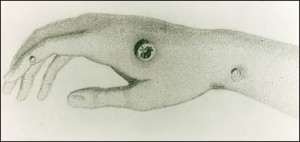
Typical appearance after a smallpox inoculation through a wound on the hand.
As the world braces for the coming flu season, with H1N1 flu preparations hurriedly taking place in tandem with “regular” efforts, I find it interesting to take a look backwards. I’m reading Paul Revere and the World He Lived In by Esther Forbes right now. If you are interested in what life was like in 1700’s Boston, her Pulitzer Prize-winning book is a must-read. She weaves tales of Paul Revere, Joseph Warren, Sam Adams, and John Hancock among others into an elegant and well-researched Revolutionary chronicle, revealing not only the history but also the life and times of these legendary characters. There is a particularly interesting section devoted to the smallpox outbreak in Boston in 1763. There were no vaccines back then, and smallpox was a disfiguring and often fatal disease. Humanity was at the mercy of most infectious diseases, and deaths in infancy and childhood were commonplace.
In December of 1763 it was acknowledged that an outbreak of smallpox had begun. The last major outbreak had occurred in 1722, during which time one half the population of Boston had contracted smallpox, and out of those infected, 1 in 6 died. The rest bore their scars for a lifetime, and pitted faces were an everyday observance.
There were no effective treatments for the disease, although a crude type of vaccination called “inoculation” was gaining support. The origin of the smallpox inoculation technique can be traced back to China, although exact dates are uncertain. It probably became common in the mid 1500’s, and spread to places such as Turkey by the 1700’s. The British Ambassador to the Ottoman Empire and his wife observed physicians in Constantinople practicing the technique, and soon it spread to Europe. The history and spread of this technique, and knowledge in general, is fascinating when compared to modern times:
The practice was introduced to the West by Lady Mary Wortley Montagu, whose husband, Edward Wortley Montagu, served as the British ambassador to the Ottoman Empire from 1716 to 1717. She witnessed inoculation being practiced by physicians in Constantinople, and was greatly impressed. She had lost a brother to smallpox and bore facial scars from the disease herself. [She had her children inoculated] She invited friends to see her daughter, including Sir Hans Sloane, the King’s physician. Sufficient interest arose that Maitland gained permission to test inoculation at Newgate Prison in exchange for the freedom of six prisoners due to be hanged, an experiment which was witnessed by a number of notable doctors. All the prisoners survived, and in 1722 the Prince of Wales’ daughters received inoculations.
The practice of inoculation slowly spread amongst the royal families of Europe, usually followed by more general adoption amongst the people.
The practice is documented in America as early as 1721, when Dr. Zabdiel Boylston, at the urging of the Reverend Cotton Mather, successfully inoculated two slaves and his own son. Mather, a prominent Boston minister, had heard a description of the African practice of inoculation from his Sudanese slave in 1706, but had been previously unable to convince local physicians to attempt the procedure. Following initial success, Boylston began performing inoculations throughout Boston, despite much controversy and at least one attempt upon his life. The effectiveness of the procedure was proven when, of the nearly three hundred people Boylston inoculated during the outbreak, only six died, whereas the mortality rate among those who contracted the disease naturally was one in six.
Inoculation was of course quite controversial, and fears ran high. Not only was Dr. Boylston threatened, mobbed on the streets, and subject to murder attempts, but the Reverend Cotton Mather, his co-promoter of inoculation, had bombs thrown at him. One landed in his home, but did not explode. On it was written: “Cotton Mather; You Dog; I’ll inoculate you with this; With a pox to you.”
Interestingly, most doctors in Boston were against inoculation in 1722, while many clergymen supported it (a counterintuitive notion in today’s world where even Popes rail against scientific truths like condoms preventing AIDS). Fortunately Dr. Boylston and Reverend Mather were brave enough to persist in their efforts.
The actual mechanism of inoculation is thus described, suffice it to say that sterile technique was not yet conceived:
Two forms of the disease of Smallpox were recognized, now known to be due to two strains of the Variola virus. Those contracting Variola Minor had a greatly reduced risk of death – 1 to 2% – compared to those contracting Variola Major with 30% mortality. Infection via inhaled viral particles in droplets spread the infection more widely than deliberate infection through a small skin wound. This smaller, localized infection is adequate to stimulate the immune system to produce specific immunity to the virus, while requiring more time to reach levels of infection likely to kill the patient. The rising immunity overwhelms the infection. So the twofold effect is to ensure that the less fatal form of the disease is the one given, and to allow the immune system the best possible head start in combating it.
Inoculation in the East was historically performed by blowing smallpox crusts into the nostril. In Britain, Europe and the American Colonies the preferred method was rubbing material from a smallpox pustule from a selected mild case (Variola minor) into a scratch between the thumb and forefinger. This would generally be performed when an individual was in normal good health, and thus at peak resistance. The recipient would develop smallpox; however, due to being introduced through the skin rather than the lungs, and possibly because of the inoculated individual’s preexisting state of good health, the small inoculum, and the single point of initial infection, the resulting case of smallpox was generally milder than the naturally-occurring form, produced far less facial scarring, and had a far lower mortality rate. As with survivors of the natural disease, the inoculated individual was subsequently immune to re-infection.
The outbreak of 1722 passed, ravaging one half the population of Boston as previously noted. When it resurfaced in large numbers in 1763 the technique of inoculation was better accepted, although still not without many opponents. What might now be called public health measures were also utilized, including the establishment of “pest houses” to quarantine those infected, forced quarantines in the home with a red flag placed outside the house, and guards placed to make sure the infected stayed home. This time the doctors of Boston were strong advocates of inoculation, with 19 physicians working tirelessly to administer the inoculations, often given for free to the poor.
The “official” statistics, gathered by the aldermen of Boston:
4,977 people received smallpox by inoculation, of whom only 46 had died, or about 1%.
699 contracted small pox naturally, and 124 had died, or about 18%, with the living often disfigured by scarring.
I find this whole historical moment (and others like it) an interesting counterpoint to our current H1N1 pandemic. Preparations for influenza are especially frantic right now, as anyone can tell from the news coverage and resources being devoted to immunization and containment. Fear of vaccination in general is still rampant, and only made worse by the “newness” of the H1N1 vaccine (which has to this date been safe in hurried trials). While no one will be standing guard outside our homes, it is recommended that people infected with the flu (who are not gravely ill and in need of hospitalization) likewise stay voluntarily quarantined at home.
Fortunately the H1N1 strain is not as lethal as it could be, nor is it as deadly as other pandemics will be in the future (such as the bird flu that never quite got off the ground a few years ago, thankfully due to poor human-to-human transmissibility). In some respects nature has given us a suitable “dry-run.” H1N1, although certainly causing deaths, popped up at the end of the winter flu season, giving us an entire Spring and Summer in the Northern Hemisphere to ready ourselves and our massive public health efforts. Of course more resources are devoted to fighting other humans than the diseases that affect our common humanity, but such is our tribal nature.
I’m getting my shots this year, with a nice clean needle, and I thank the brave tides before my time, upon whose accumulated knowledge and scientific truths we somehow sustain a planet of 6 billion humans, and can reasonably hope to live into old age as Paul Revere did. And don’t forget to read Esther Forbes masterpiece that won the Pulitzer Prize in 1942, and support a great bookstore.
A good resource for more current information is at www.flu.gov.
I think you’re being unduly harsh on the resistance to inoculation. Let’s face it, this was anecdotal treatment, where you had to have some “leap of faith” to trust someone that if they gave you smallpox (ie, 100% infection rate), you might be saved from dying.
This is quite, quite different from the eventual smallpox vaccination we all went through years ago, with a simple cutaneous inoculation using cowpox virus.
What if someone proposed inoculating you with HIV?
Not sure how I’m being unduly harsh… except for noting that “fear” was present then, and is still present now in terms of much safer immunization.
I would have been quite scared getting the inoculation back in that day, even though it seems there was some good accumulated evidence by 1763 that it was worth the risk. Shows you the quantum leaps that have been made in surveillance, record-keeping, and clinical trials.
No thanks on the HIV inoculation… that’s really not analogous, and adds a certain “edge” to your comment that’s surprising.
An interesting question:
Was getting the smallpox inoculation a rational choice for a Bostonian in 1763?
They could have known that in 1722, during the last major smallpox breakout, 50% of the population contracted smallpox and 1 in 6 died, the rest were scarred to varying degrees. Cumulative risk of dying from smallpox –> 1/2 x 1/6 = 1/12 chance of dying
In 1722, Dr. Boylston observed that of the 300 people he inoculated, only 6 died (see above). But if you got the inoculation you had a 100% infection rate as you noted.
Cumulative risk of dying from inoculation –> 1/1 x 6/300 = 1/50 chance of dying.
Rationally, you would chose a 1/50 chance of dying over a 1/12, although I still understand the fear of 1/12 dying. In modern times, with seemingly unproven vaccine fears, a similar accounting of relative risks seems like a good idea.
If you want a first hand account of smallpox innoculation in colonial Boston read the letters of John and Abagail Adams. Some of the earliest letters between them are from the time before they were married when John went into the city to be innoculated and wrote to Abagail about the experience. Later while John was off serving in Congress during the war Abagail took all of the children into Boston to be innoculated and wrote to John about it.
I saw the John Adams movie on HBO and they dramatized Abagail’s inoculation of the children.
The doctor brought around a poor soul in the back of a wagon. He had lots of juicy pustules and the doctor extracted some of that to do the children. Quite a ways from the clean little glass vile they use today.